

This is a result of impaired platelet function, inhibition of the clotting factors, and inappropriate activation of clot breakdown.8
#TRAUMA TRIAD OF DEATH SERIES#
(See Table 2.) Of particular concern is the effect of hypothermia on the coagulation system.8 The coagulation system is a temperature- and pH-dependent series of complex enzymatic reactions that result in the formation of blood clots to stop both internal and external hemorrhage.Ĭoagulopathy is the term used to describe a broad group of disease states in which there is an impaired ability of this coagulation system to synthesize blood clots.5 It’s been repeatedly demonstrated that as a patient’s core temperature decreases, so does the body’s ability to stop bleeding. (See Table 1–below.)Įven mild hypothermia in a trauma patient can result in devastating physiologic consequences. In a study of 71 trauma victims, a core temperature < 32 degrees C was associated with 100% mortality independent of the presence of shock, injury severity or volume of fluid resuscitation.7 Because hypothermia in a trauma patient predicts such a poor outcome, the traditional classification system of hypothermia has been revised for use in this vulnerable patient population. At highest risk were those patients older than 65 and those who had been entrapped.6 In addition, hypothermia in trauma has been associated with a significantly increased mortality compared to patients with the same body temperature from environmental exposure alone. Normal human body temperature is 35.6-37.8 degrees C with hypothermia being defined as a core temperature < 35 degrees C.5 In one study, it was found that almost half of EMS-transported trauma patients had a temperature < 36 degrees C on arrival to the ED.6 Important to note is that there was no association between season of the year and frequency of hypothermia. Left untreated, hypothermia, acidosis and coagulopathy bring about and propagate each other, eventually resulting in a predictable but irreversible progression toward death. This understanding should serve as the cornerstone for all interventions provided to the bleeding trauma patient.
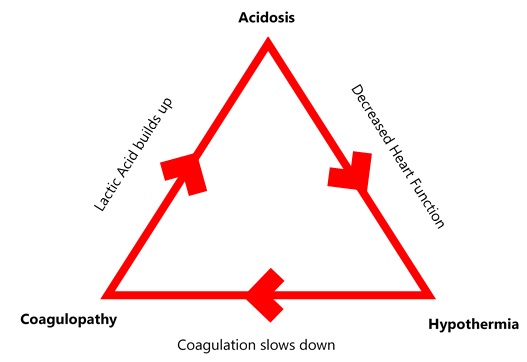
Today, we recognize that to successfully resuscitate the critically ill trauma patient, all emergency providers must have a firm understanding of the lethal triad. Authors of the research suggested treatment of hypothermia, acidosis and coagulopathy in trauma requires as much attention as the traditionally emphasized surgical management of injuries.4 In 1982, a study described a “bloody vicious cycle” in which hemorrhage and tissue injury cause this predictable triad of complicating factors.4 Ultimately, this triad resulted in worsening hemorrhage and eventual death. The lethal triad of hypothermia, acidosis and coagulopathy has been recognized as a significant cause of death in patients with traumatic injuries. 1 cause of death in the United States.1 Of these deaths, hemorrhage accounts for up to 40% and remains as the leading preventable cause of trauma-related death.2,3 This is especially apparent in the young–for those aged 1-44 years old, trauma is the No. As you and your partner begin your rapid trauma assessment, obtain vital signs, and prepare for rapid packaging and transport to the trauma center 20 minutes away, you know this young man is on the brink of death.ĭespite great advancements in trauma care over the past 30 years, trauma is still one of the leading causes of death in any age group.

He’s nearly unconscious but breathing spontaneously. On arrival you find a 25-year-old male lying on the street in a rapidly expanding pool of blood. En route, police notify you the scene is safe and there’s a single patient bleeding profusely from multiple extremity wounds. on a Saturday night when you’re dispatched to a local nightclub for reports of a young male who’s suffered multiple gunshot wounds.


 0 kommentar(er)
0 kommentar(er)
